Impacts of sleep disorders on the quality of life of children and adolescents
DOI:
https://doi.org/10.14295/bjs.v5i2.834Keywords:
sleep, sleep disorders, children, adolescents, quality of lifeAbstract
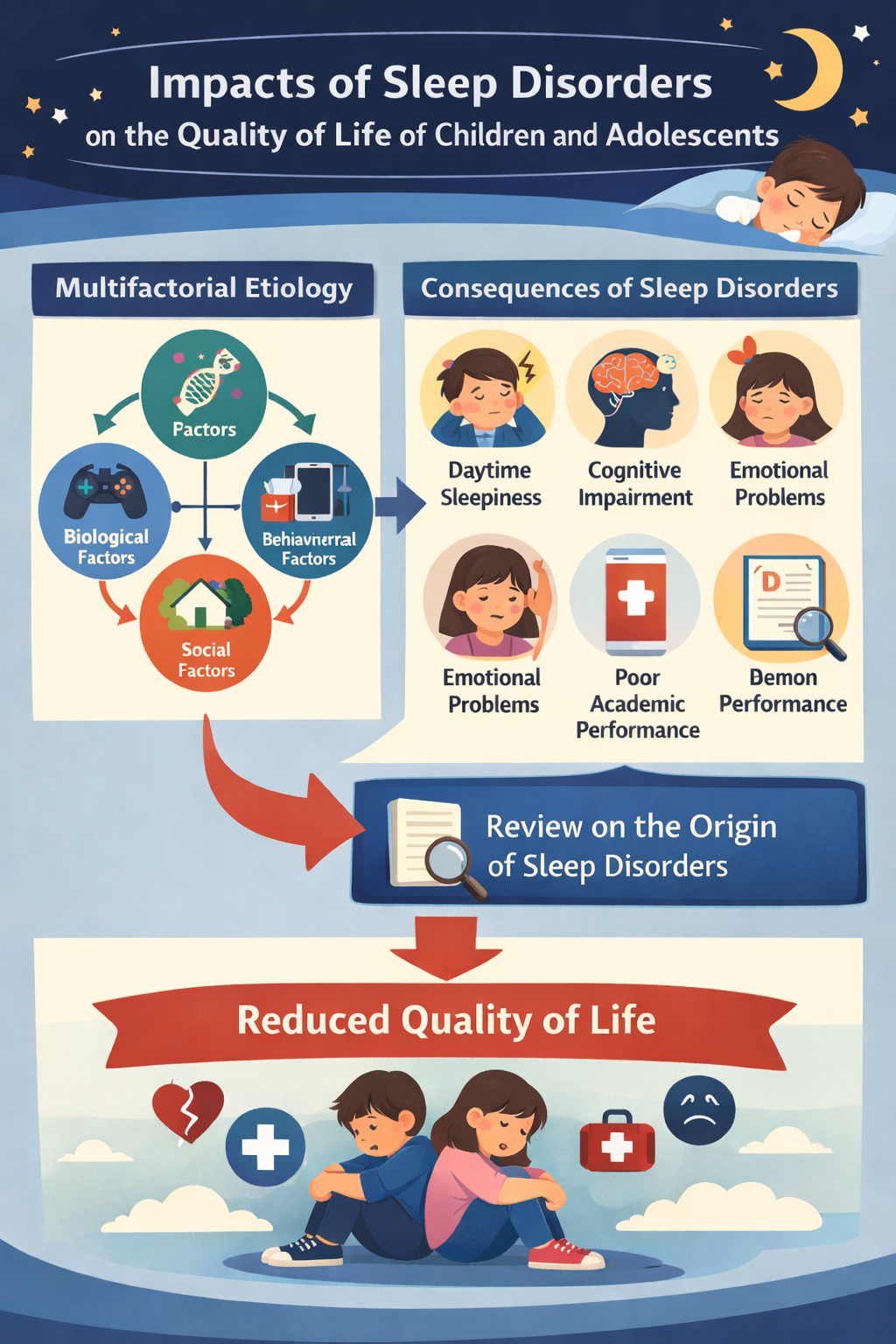
Sleep is an essential physiological process for the proper physical, cognitive, and emotional development of children and adolescents. Sleep disorders, including insomnia, respiratory disturbances, and circadian rhythm dysregulation, are highly prevalent in this population and are associated with negative impacts on quality of life. To analyze factors associated with sleep disorders in children and adolescents and their effects on development and quality of life. This is an integrative literature review based on articles published between 2013 and 2025 in the SciELO, LILACS, Scopus, and MEDLINE databases, using the descriptors “sleep,” “sleep disorders,” “insomnia,” “sleep apnea,” “child health,” and “adolescent.” Studies published in Portuguese, Spanish, or English were included, totaling ten selected articles, of which four were literature reviews, and four were observational studies. The main factors associated with sleep disorders were excessive use of electronic devices, unhealthy dietary habits, unfavorable school schedules, sociogeographic factors, and secondary conditions, such as ASD. Persistent sleep disorders were associated with cognitive impairment, behavioral changes, emotional compromise, and an increased risk of chronic diseases, such as asthma. Sleep disorders in children and adolescents have a multifactorial etiology and can significantly compromise quality of life and overall development. Preventive strategies and multidisciplinary interventions, combined with public health policies aimed at promoting healthy sleep, are essential to reduce their impact.
References
Ahmed, I., & Thorpy, M. (2010). Clinical features, diagnosis and treatment of narcolepsy. Clinics in Chest Medicine, 31(2), 371-381. https://doi.org/10.1016/j.ccm.2010.02.003
Albertini, M. L., Spoto, G., Ceraolo, G., Fichera, M. F., Consoli, C., Nicotera, A. G., & Di Rosa, G. (2025). Sleep disorders in children with autism spectrum disorder: developmental impact and intervention strategies. Brain Sciences, 15(9), 983. https://doi.org/10.3390/brainsci15090983
Associação Brasileira do Sono. (2025). Conselho de Psicologia do Sono. 1. ed., 2023. Available at: https://absono.com.br/wp-content/uploads/2023/10/abs-cartilha-sono-crianca-adolescente-out2023.pdf. Accessed on: Oct 7, 2025.
American Academy of Sleep Medicine. (2025). International classification of sleep disorders (ICSD). 3. ed., 2014. Disponível em: http://www.aasmnet.org/library/default.aspx?id=9. Acesso em: 07 out. 2025.
Berger, H. (1931). Über das elektrenkephalogramm des menschen: dritte mitteilung. Archiv für Psychiatrie und Nervenkrankheiten, 94(1), 16-60. https://doi.org/10.1007/BF01835097
Berry, R. B. et al. (2017). The AASM manual for the scoring of sleep and associated events: rules, terminology and technical specifications. In: American Academy of Sleep Medicine (Ed.). Scoring manual version 2.4. Darien, 1-89.
Bryant, P. A., Trinder, J., & Curtis, N. (2004). Sick and tired: does sleep have a vital role in the immune system? Nature Reviews Immunology, 4(6), 457-467. https://doi.org/10.1038/nri1369
Bruni, O., & Angriman, M. (2015). L’insonnia in eta evolutiva. Médico Bambino, 34, 224-233.
Ehsan, Z., Ishman, S. L., Kimball. T. R., Zhang, N., Zou, Y., & Amin, R. S. (2017). Longitudinal cardiovascular outcomes of sleep disordered breathing in children: a meta-analysis and systematic review. Sleep, 40(3). https://doi.org/10.1093/sleep/zsx015
El Halal, C. S., Nunes, M. L. (2025). Sleep disorder assessment in children and adolescents with neurodevelopmental disorders. Jornal de Pediatria, 101(supl. 1), 101441. https://doi.org/10.1016/j.jped.2025.101441
Ercole, F. F., Melo, L. S. D., & Alcoforado, C. L. G. C. (2014). Revisão integrativa versus revisão sistemática. Revista Mineira de Enfermagem, 18(1), 9-12. https://doi.org/10.5935/1415-2762.20140001
Frigeri, M. (2014). SciELO: quinze anos de parceria com os periódicos científicos. Ciência e Cultura, 66(1). http://dx.doi.org/10.21800/S0009-67252014000100006
Gradisar, M., & Crowley, S. J. (2013). Delayed sleep phase disorder in youth. Current Opinion in Psychiatry, 26(6), 580-585. https://doi.org/10.1097/YCO.0b013e328365a1d4
Grime, C., & Tan, H. L. (2015). Sleep disordered breathing in children. The Indian Journal of Pediatrics, 82(10), 945-955. https://doi.org/10.1007/s12098-015-1857-5
Hirshkowitz, M., Whiton, K., Albert, S. M., Alessi, C., Bruni, O., DonCarlos, L., Hazen, N., Herman, J., Katz, E. S., Kheirandish-Gozal, L., Neubauer, D. N., O’Donnell, A. E., Ohayon, M., Peever, J., Rawding, R., Sachdeva, R. C., Setters, B., Vitiello, M., Ware, J. C., & Hillard, P. J. A. (2015). National sleep foundation’s sleep time duration recommendations: methodology and results summary. Sleep Health, 1(1), 40-43. https://doi.org/10.1016/j.sleh.2014.12.010
Kleitman, N., & Engelmann, T. G. (1953). Sleep characteristics of infants. Journal of Applied Physiology, 6(5), 269-282. https://doi.org/10.1152/jappl.1953.6.5.269
Kotagal, S. (2009). Parasomnias in childhood. Sleep Medicine Reviews, 13(2), 157-168. https://doi.org/10.1016/j.smrv.2008.09.005
Liu, J., Ji, X., Rovit, E., Pitt, S., & Lipman, T. (2024). Childhood sleep: assessments, risk factors, and potential mechanisms. World Journal of Pediatrics, 20, 105-121. https://doi.org/10.1007/s12519-022-00628-z
Luboshitzky, R. (2000). Endocrine activity during sleep. Journal of Pediatric Endocrinology & Metabolism, 13(1), 13-20.
Marcus, C. L., Brooks, L. J., Ward, S. D., Draper, K. A., Gozal, D., Halbower, A. C., Jones, J., Lehmann, C., Schechter, S., Sheldon, S., Shiffman, R. N., & Spruyt, K. (2012). Diagnosis and management of childhood obstructive sleep apnea syndrome. Pediatrics, 130(3), e714-755. https://doi.org/10.1542/peds.2012-1672
Martinez, D., Lenz, M. O. C., & Menna-Barreto, L. (2008). Diagnosis of circadian rhythm sleep disorders. Jornal Brasileiro de Pneumologia, 34(3), 173-180. https://doi.org/10.1590/S1806-37132008000300008
Maski, K., & Owens, J. A. (2016). Insomnia, parasomnias, and narcolepsy in children: clinical features, diagnosis, and management. Lancet Neurology, 15(11), 1170-1181.
Mason, G. M., Lokhandwala, S., Riggins, T., & Spencer, R. M. C. (2021). Sleep and human cognitive development. Sleep Medicine Reviews, 57, 101472. https://doi.org/10.1016/j.smrv.2021.101472
Matwiyoff, G., & Lee-Chiong, T. (2010). Parasomnias: an overview. IJMR - Indian Journal of Medical Research, 131, 333-337.
Mendes, K. D. S., Silveira, R. C. C. P., & Galvão, C. M. (2008). Revisão integrativa: método de pesquisa para a incorporação de evidências na saúde e na enfermagem. Texto Contexto Enferm, 17(4), 758-764. https://doi.org/10.1590/S0104-07072008000400018
Nielsen, T. (2017). The stress acceleration hypothesis of nightmares. Frontiers in Neurology, 8, 201. https://doi.org/10.3389/fneur.2017.00201
Nixon, G. M., Davey, M. (2015). Sleep apnoea in the child. Australian Family Physician, 44(6), 352-355.
Nunes, M. L. (2002). Distúrbios do sono. Jornal de Pediatria, 78(suppl 1), S63-S72. https://doi.org/10.1590/S0021-75572002000700010
Nunes, M. L., & Bruni, O. (2015). Insomnia in childhood and adolescence: clinical aspects, diagnosis, and therapeutic approach. Jornal de Pediatria, 91(suppl 1), S26-S35. https://doi.org/10.1016/j.jped.2015.08.006
Ouyang, A., Lin, X., Zhang, T., Li, J., Wang, L., Cao, Z., Diao, X., He, W., Dong, Q., Jiang, J., & Fang, P. (2026). The impact of sleep deprivation on dynamic functional connectivity of the brain: Based on alertness task performance. Brain Research Bulletin, 235, 111712. https://doi.org/10.1016/j.brainresbull.2025.111712
Pereira, É. F., Teixeira, C. S., & Santos, A. (2012). Qualidade de vida: abordagens, conceitos e avaliação. Revista Brasileira de Educação Física e Esporte, 26(2), 241-250. https://doi.org/10.1590/S1807-55092012000200007
Picchietti, D. L, Bruni, O., de Weerd, A., Durmer, J. S., Kotagal, S., Owens, J. A., & Simakajornboon N. (2013). Pediatric restless legs syndrome diagnostic criteria: an update by the International Restless Legs Syndrome Study Group. Sleep Medicine, 14(12), 1253-1259. https://doi.org/10.1016/j.sleep.2013.08.778
Owens, J., & Group ASW, & Adolescence CO. (2014). Insufficient sleep in adolescents and young adults: an update on causes and consequences. Pediatrics, 134(3), e921-e932. https://doi.org/10.1542/peds.2014-1696
Ribeiro, M. (2023). Como o sono impacta o desenvolvimento infantil. Drauzio. Available at: https://drauziovarella.uol.com.br/pediatria/como-o-sono-impacta-o-desenvolvimento-infantil/. Accessed on: Jan 8, 2026.
Roeths, T., & Roth, T. (2000). Sleep-wake state and memory function. Sleep, 23(supl. 3), S64-S68.
Sateia, M. J. (2014). International classification of sleep disorders-third edition: highlights and modifications. Chest, 146(5), 1387-1394. https://doi.org/10.1378/chest.14-0970
Schredl, M., Fricke-Oerkermann, L., Mitschke, A., & Lehmkuhl, G. (2009). Longitudinal study of nightmares in children: stability and effect of emotional symptoms. Child Psychiatry and Human Development, 40(3), 439-449. https://doi.org/10.1007/s10578-009-0136-y
Simakajornboon, N., Kheirandish-Gozal, L., & Gozal, D. (2009). Diagnosis and management of restless legs syndrome in children. Sleep Medicine Reviews, 13(2), 149-156. https://doi.org/10.1016/j.smrv.2008.12.002
Simões, A. D., Júnior, Á. N. M., Oliveira, A. B. S., Pereira, A. C. P., Figueiredo, B. Q., Pinheiro, F. E. S., & Lopes, L. F. P. (2022). Main sleep disorders and their impacts on human quality of life: a systematic literature review. Research Society and Development, 11(5), e38411528457. https://doi.org/10.33448/rsd-v11i5.28457
Sousa, L. M. M., Marques-Vieira, C. M. A., Severino, S. S., & Antunes, A. V. (2017). A metodologia de revisão integrativa da literatura em enfermagem. Revista Investigação em Enfermagem, 17-26.
Stallman, H. M., & Kohler, M. (2016). Prevalence of sleepwalking: a systematic review and meta-analysis. PLoS One, 11(11), e0164769. https://doi.org/10.1371/journal.pone.0164769
Tavares, A., Zancanella, E., Genta, P. R., & Poyares, D. (2023). Medicina do sono: diagnóstico e manejo. Grupo A, Porto Alegre: Artmed.
Vyazovskiy, V. V. (2015). Sleep, recovery, and metaregulation: explaining the benefits of sleep. Nature and Science of Sleep, 7(1), 171-184. https://doi.org/10.2147/NSS.S54036
Wittert, G. (2014). The relationship between sleep disorders and testosterone. Current Opinion in Endocrinology Diabetes and Obesity, 21(3), 239-243. https://doi.org/10.1097/MED.0000000000000069
Zhang, M-M., Ma, Y., Du, L-T., Wang, K., Zhu, W., Sun, Y-H., Lu, L., Bao, Y-P., & Li, S-X. (2022). Sleep disorders and non-sleep circadian disorders predict depression: A systematic review and meta-analysis of longitudinal studies. Neuroscience & Biobehavioral Reviews, 134, 104532. https://doi.org/10.1016/j.neubiorev.2022.104532
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2026 Gabriela Martins, Renata Dellalibera-Joviliano

This work is licensed under a Creative Commons Attribution 4.0 International License.
Authors who publish with this journal agree to the following terms:
1) Authors retain copyright and grant the journal right of first publication with the work simultaneously licensed under a Creative Commons Attribution License that allows others to share the work with an acknowledgement of the work's authorship and initial publication in this journal.
2) Authors are able to enter into separate, additional contractual arrangements for the non-exclusive distribution of the journal's published version of the work (e.g., post it to an institutional repository or publish it in a book), with an acknowledgement of its initial publication in this journal.
3) Authors are permitted and encouraged to post their work online (e.g., in institutional repositories or on their website) prior to and during the submission process, as it can lead to productive exchanges, as well as earlier and greater citation of published work.