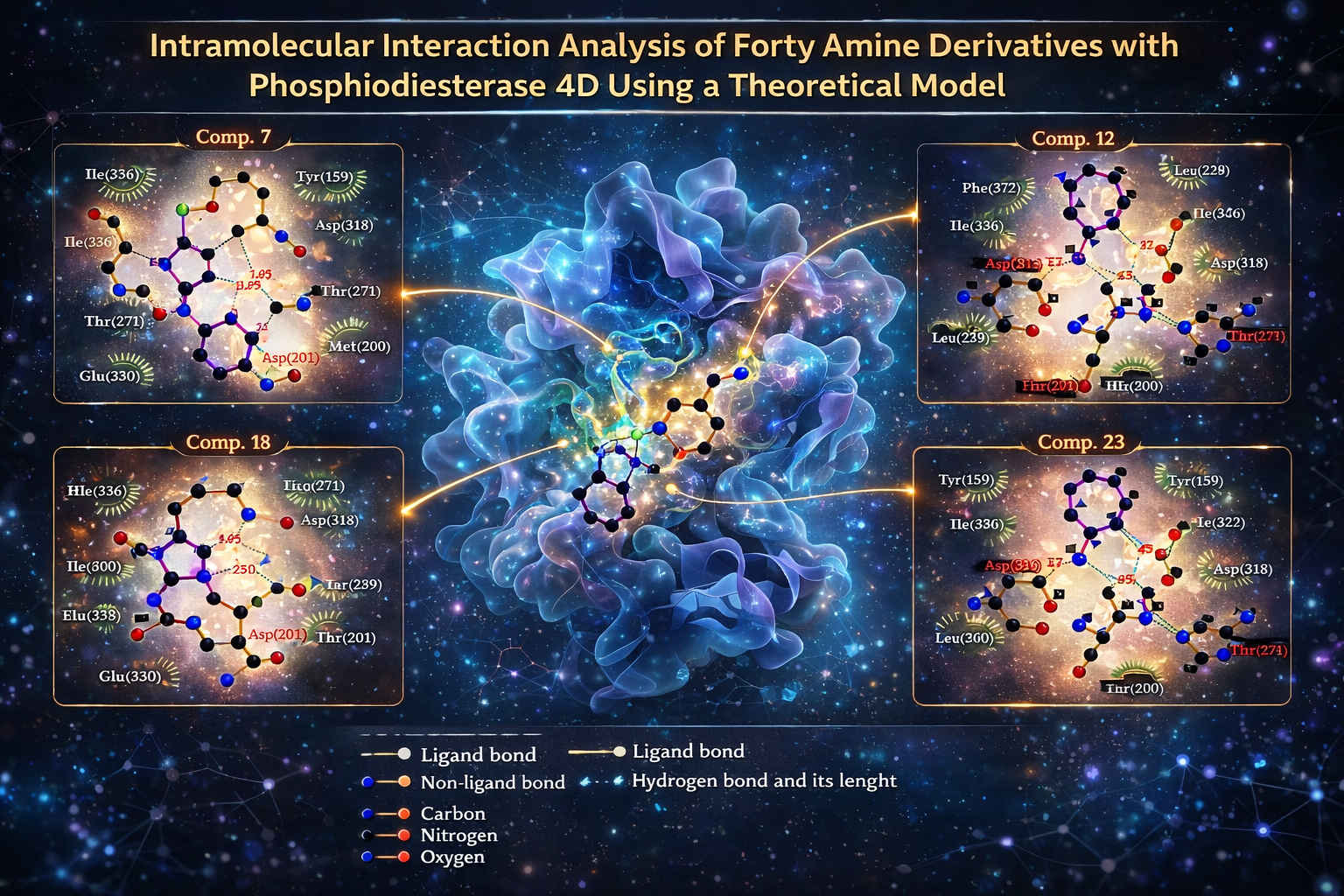
Intramolecular interaction analysis of forty amine derivatives with phosphodiesterase 4D using a theoretical model
DOI:
https://doi.org/10.14295/bjs.v5i3.825Keywords:
amino derivatives, heart failure, phosphodiesteraseAbstract
Several drugs, such as zatolmilast, orismilast, lotamilast, and GSK256066 (phosphodiesterase inhibitors) have been used to treat chronic heart failure. However, some of these drugs can produce different secondary effects such as arrhythmia, nausea, and vomiting. In the search for a new therapeutic alternative to treat chronic heart failure, this study aimed to characterize the interaction of some amino derivatives (1-40) with phosphodiesterase 4D using the 3iak protein as a theoretical tool in the DockingServer program. Besides, zatolmilast, orismilast, lotamilast, and GSK256066 were used as controls. The results showed differences in the interaction of amino derivatives with the 3iak protein surface compared with zatolmilast, orismilast, lotamilast, and GSK256066. Other data indicate that the inhibition constant for amino derivatives 7, 12, 15, 18, and 33 was lower compared with the controls. All these data suggest that compounds 7, 12, 15, 18, and 33 could act as phosphodiesterase 4D inhibitors. These data suggest that amino derivatives of phosphodiesterase 4D could be a good therapeutic alternative to treat heart failure.
References
Akama, T., Shida, Y., Sugaya, T., Ishida, H., Gomi, K., & Kasai, M. (1996). Novel 5-aminoflavone derivatives as specific antitumor agents in breast cancer. Journal of Medicinal Chemistry, 39(18), 3461-3469. https://doi.org/10.1021/jm950938g
Askerova, U. (2023). Prediction of acute toxicity for (Z)-3-(2-phenylhydrazinylidene) benzofuran-2 (3H)-one and its derivatives for rats using GUSAR program. New Materials, Compounds and Applications, 7(1), 50-56.
Aune, D., Schlesinger, S., Norat, T., & Riboli, E. (2019). Tobacco smoking and the risk of heart failure: A systematic review and meta-analysis of prospective studies. European Journal of Preventive Cardiology, 26(3), 279-288. https://doi.org/10.1177/2047487318806658
Batchelder, K., & Mayosi, B. M. (2005). Pentoxifylline for heart failure: a systematic review. South African Medical Journal, 95(3).
Boswell-Smith, V., Spina, D., Oxford, A., Comer, M., Seeds, E., & Page, C. P. (2006). The Pharmacology of Two Novel Long-Acting Phosphodiesterase 3/4 Inhibitors, RPL554 [9, 10-Dimethoxy-2 (2, 4, 6-trimethylphenylimino)-3-(N-carbamoyl-2-aminoethyl)-3, 4, 6, 7-tetrahydro-2 H-pyrimido [6, 1-a] isoquinolin-4-one] and RPL565 [6, 7-Dihydro-2-(2, 6-diisopropylphenoxy)-9, 10-dimethoxy-4 H-pyrimido [6, 1-a] isoquinolin-4-one]. The Journal of Pharmacology and Experimental Therapeutics, 318(2), 840-848.https://doi.org/10.1124/jpet.105.099192
Bragazzi, N., Zhong, W., Shu, J., Abu-Much, A., Lotan, D., Grupper, A., & Dai, H. (2021). Burden of heart failure and underlying causes in 195 countries and territories from 1990 to 2017. European Journal of Preventive Cardiology, 28(15), 1682-1690. https://doi.org/10.1093/eurjpc/zwaa147
Bushueva, I., & Parchenko, M. (2024). Acute toxicity of 5-((5-bromofuran-2-yl)-4-methyl-3-thioheptyl)-1, 2, 4-triazole. Art of Medicine, 40-44.
Champion, S., Lapidus, N., Cherié, G., Spagnoli, V., Oliary, J., & Solal, A. C. (2014). Pentoxifylline in heart failure: a meta‐analysis of clinical trials. Cardiovascular Therapeutics, 32(4), 159-162. https://doi.org/10.1111/1755-5922.12076
Cuffe, M., Califf, R., Adams Jr, K., Benza, R., Bourge, R., & Colucci, W. (2002). Short-term intravenous milrinone for acute exacerbation of chronic heart failure: a randomized controlled trial. Journal of American Medical Association, 287(12), 1541-1547. https://doi.org/10.1001/jama.287.12.1541.
Di Muzio, E.Toti,D.,&Polticelli, F. (2017). DockingApp: a user friendlyinterfaceforfacilitated docking simulations with AutoDock Vina. Journal of Computer-Aided Molecular Design, 31, 213-218
Dix, D., Houck, K., Martin, M., Richard, A., Setzer, R., & Kavlock, R. (2007). The ToxCast program for prioritizing toxicity testing of environmental chemicals. Toxicological Sciences, 95(1), 5-12.
Figueroa-Valverde, L., Rosas-Nexticapa, M., Alvarez-Ramirez, M., Aguilar-Sanchez, E., Mateu-Armad, M., & Bonilla-Zavaleta, E. (2024). Interaction of some chalcone derivatives with calcium channels using a theoretical model. Brazilian Journal of Science, 3(11), 1-15. https://doi.org/10.14295/bjs.v3i11.658
Fu, J., Su, C., Ge, Y., Ao, Z., Xia, L., Chen, Y., Yang, Y., Chen, S., Xu, R., Yang, X., Huang, K., & Fu, Q. (2025). PDE4D inhibition ameliorates cardiac hypertrophy and heart failure by activating mitophagy. Redox Biology, 81. https://doi.org/10.1016/j.redox.2025.103563
Harren, T., Gutermuth, T., Grebner, C., Hessler, G., & Rarey, M. (2024). Modern machine-learning for binding affinity estimation of protein-ligand complexes: Progress, opportunities, and challenges. Wiley Interdisciplinary Reviews: Computational Molecular Science, 14(3), e1716. https://doi.org/10.1002/wcms.1716
Huang, C., Park, J., Liu, I., Lee, J., Kohan, S., Mefford, M., & Lee, M. S. (2024). Effectiveness and safety of early treatment with spironolactone for new‐onset acute heart failure. Journal of Hospital Medicine, 19(4), 267-277. https://doi.org/10.1002/jhm.13317
Katsiki, N., Doumas, M., & Mikhailidis, D. (2016). Lipids, statins and heart failure: an update. Current Pharmaceutical Design, 22(31), 4796-4806
Khalifa, M. (2018). Recent Developments and Biological Activities of 2-Aminothiazole Derivatives. Acta Chimica Slovenica, 65(1).
Khan, M., Shahid, I., Bennis, A., Rakisheva, A., Metra, M., & Butler, J. (2024). Global epidemiology of heart failure. Nature Reviews Cardiology, 1-18.
Kim, K., Kim, H., Hwang, I., Cho, H., Je, N., Kwon, O., & Sohn, D. (2015). PDE 5 inhibition with udenafil improves left ventricular systolic/diastolic functions and exercise capacity in patients with chronic heart failure with reduced ejection fraction; A 12-week, randomized, double-blind, placebo-controlled trial. American Heart Journal, 169(6), 813-822. https://doi.org/10.1016/j.ahj.2015.03.018
Klopman, G., & Rosenkranz, H. (1995). Toxicity estimation by chemical structure analysis: the TOX II program. Toxicology Letters, 79(1-3), 145-155. https://doi.org/10.1016/0378-4274(95)03366-S
Laonigro, I., Correale, M., Di Biase, M., & Altomare, E. (2009). Alcohol abuse and heart failure. European Journal of Heart Failure, 11(5), 453-462. https://doi.org/10.1093/eurjhf/hfp037
Le Jemtel, T., Keung, E., Ribner, H., Davis, R., Wexler, J., Blaufox, M., & Sonnenblick, E. (1980). Sustained beneficial effects of oral amrinone on cardiac and renal function in patients with severe congestive heart failure. The American Journal of Cardiology, 45(1), 123-129.https://doi.org/10.1016/0002-9149(80)90229-5
Lee, C., Lee, H., Yoon, M., Chun, K., Kong, M., Jung, M., & Kang, S. (2024). Heart failure statistics 2024 update: A report from the Korean society of heart failure. International Journal of Heart Failure, 6(2), 56. https://doi.org/10.36628%2Fijhf.2024.0010
Levitt, D. (2002). PKQuest: a general physiologically based pharmacokinetic model. Introduction and application to propranolol. BMC Clinical Pharmacology, 2(1), 1-21.
Liu, M., Lin, T., Cory, J., Cory, A., & Sartorelli, A. (1996). Synthesis and biological activity of 3-and 5-amino derivatives of pyridine-2-carboxaldehyde thiosemicarbazone. Journal of Medicinal Chemistry, 39(13), 2586-2593. https://doi.org/10.1021/jm9600454
Lu, W., Zhang, J., Huang, W., Zhang, Z., Jia, X., Wang, Z., & Zheng, S. (2024). DynamicBind: predicting ligand-specific protein-ligand complex structure with a deep equivariant generative model. Nature Communications, 15(1), 1071.
Maggioni, A., Latini, R., Carson, P.,Singh, S., Barlera, S., & Glazer, R. (2005). Valsartan reduces the incidence of atrial fibrillation in patients with heart failure: results from the Valsartan Heart Failure Trial (Val-HeFT). American Heart Journal, 149(3), 548-557.
Martin, S., Aday, A., Almarzooq, Z., Anderson, C., Arora, P., & Avery, C. (2024). 2024 heart disease and stroke statistics: a report of US and global data from the American Heart Association. Circulation, 149(8), e347-e913. https://doi.org/10.1161/CIR.0000000000001209
Masarone, D., Kittleson, M., Pollesello, P., Marini, M., Iacoviello, M., Oliva, F., & Pacileo, G. (2022). Use of levosimendan in patients with advanced heart failure: an update. Journal of Clinical Medicine, 11(21), 6408. https://www.mdpi.com/2077-0383/11/21/6408#
Nielsen, R., Pryds, K., Olesen, K., Mortensen, M., Gyldenkerne, C., Nielsen, J., & Maeng, M. (2024). Coronary artery disease is a stronger predictor of all‐cause mortality than left ventricular ejection fraction among patients with newly diagnosed heart failure: Insights from the WDHR. Journal of the American Heart Association,13(14), e9771. https://doi.org/10.1161/JAHA.123.033938
Ohkuma, T., Komorita, Y., Peters, S., & Woodward, M. (2019). Diabetes as a risk factor for heart failure in women and men: a systematic review and meta-analysis of 47 cohorts including 12 million individuals. Diabetologia, 62, 1550-1560.
Packer, M., Carver, J., Rodeheffer, R., Ivanhoe, R., DiBianco, R., & Zeldis, S. (1991). Effect of oral milrinone on mortality in severe chronic heart failure. New England Journal of Medicine, 325(21), 1468-1475. https://doi.org/10.1056/NEJM199111213252103
Packer, M., Carver, J., Rodeheffer, R., Ivanhoe, R., DiBianco, R., & Zeldis, S. (1991). Effect of oral milrinone on mortality in severe chronic heart failure. New England Journal of Medicine, 325(21), 1468-1475. https://doi.org/10.1056/NEJM19911121325210
Plewczynski, D., Philips, A., Grotthuss, M., Rychlewski, L., & Ginalski, K. (2014). HarmonyDOCK: the structural analysisof poses in protein-ligand docking. Journal of Computational Biology, 21(3), 247-256. https://doi.org/10.1089/cmb.2009.0111
Prasetyawan, F., Saristiana, Y., Mildawati, R., Rhomah, E., Fadel, M., & Besan, E. (2025). Pharmacokinetics and Druglikeness of Amoxicillin Drug using SwissADME. Multicore International Journal of Multidisciplinary, 1(2), 67-75.
Qiao, Z., Nie, W., Vahdat, A., Miller III, T. F., & Anandkumar, A. (2024). State-specific protein–ligand complex structure prediction with a multiscale deep generative model. Nature Machine Intelligence, 6(2), 195-208.
Riniker, S., Christ, C., Hansen, H., Hünenberger, P., Oostenbrink, C., Steiner, D., & Van-Gunsteren, W. (2011). Calculation of relativefreeenergyforligand-protein binding, solvation, and conformational transitions using the GROMOS software. The Journal of Physical Chemistry B, 115(46), 13570-13577. https://doi.org/10.1021/jp204303a
Saleh, M., Saleh, J., Al-Badrany, K., Dalaf, A., Najm, R., & Talluh, A. (2024). Preparation and evaluation of the biological activity of a 2-amino pyran ring using a solid base catalyst. Central Asian Journal of Medical and Natural Science, 5(4), 130-138.
Sanada, S., Asanuma, H., Koretsune, Y., Watanabe, K., Nanto, S., Awata, N., & Hori, M. (2007). Long-term oral administration of dipyridamole improves both cardiac and physical status in patients with mild to moderate chronic heart failure: a prospective open-randomized study. Hypertension Research, 30(10), 913-919.
Seiler, N. (2003). Thirty years of polyamine-related approaches to cancer therapy. Retrospect and prospect. Part 2. Structural analogues and derivatives. Current Drug Targets, 4(7), 565-585. https://doi.org/10.2174/1389450033490876
Shaku, S., Bakare-Odunola, M., Musa, A., Yakasai, I., Garba, M., & Adzu, B. (2020). Effect of dihydro-artemisinin on the pharmacokinetics of gliclazide in diabetic subjects. International Journal of Biological and Chemical Sciences,14(6), 2267-2276. https://doi.org/10.33263/BRIAC133.266
Sherstnev, I., Judina, A., Luciani, G. B., Ghigo, A., Hirsch, E., & Gorelik, J. (2025). Role of PDE4 family in cardiomyocyte physiology and heart failure. Cells, 14(6), 460. https://doi.org/10.3390/cells14060460
Sicak, Y. (2021). Design and antiproliferative and antioxidant activities of furan-based thiosemicarbazides and 1, 2, 4-triazoles: their structure-activity relationship and SwissADME predictions. Medicinal Chemistry Research, 30(8), 1557-156
Slivnick, J., & Lampert, B. (2019). Hypertension and heart failure. Heart Failure Clinics,15(4), 531-541. https://doi.org/10.1016/j.hfc.2019.06.007
T
rosset, J., & Scheraga, H. (1999). PRODOCK: software package for protein modeling and docking. Journal of Computational Chemistry, 20(4), 412-427. https://doi.org/10.1002/(SICI)1096-987X(199903)20:4%3C412:AID-JCC3%3E3.0.CO;2-N
Walker, K., Boots, M., Stubbins, J., Rogers, M., & Davis, C. (1983). 1-(4-Aminobenzyl)-and 1-(4-aminophenyl) isoquinoline derivatives: synthesis and evaluation as potential irreversible cyclic nucleotide phosphodiesterase inhibitors. Journal of Medicinal Chemistry, 26(2), 174-181. https://doi.org/10.1021/jm00356a011
Waters, M., & Auletta, A. (1981). The GENE-TOX program: genetic activity evaluation. Journal of Chemical Information and Computer Sciences, 21(1), 35-38. https://doi.org/10.1021/ci00029a007
Wilsmhurst, P., & Webb-Peploe, M. (1983). Side effects of amrinone therapy. Heart, 49(5), 447-451. https://doi.org/10.1136/hrt.49.5.447
Wu, E., El Ahmadieh, T., Kafka, B., Davies, M., Aoun, S., & White, J. A. (2018). Milrinone-associated cardiomyopathy and arrhythmia in cerebral vasospasm. World Neurosurgery, 114, 252-256. https://doi.org/10.1016/j.wneu.2018.03.151
Yan, Y., Zhang, X., Xiao, Y., Shen, X., Jian, Y.., Wang, Y., & Liu, X. (2022). Design and synthesis of a 2-amino-pyridine derivative as a potent CDK8 inhibitor for anti-colorectal cancer therapy. Journal of Medicinal Chemistry, 65(19), 13216-13239. https://doi.org/10.1021/acs.jmedchem.2c01042
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2026 Magdalena Álvarez-Ramírez, Marcela Rosas-Nexticapa, María Virginia Mateu-Armad

This work is licensed under a Creative Commons Attribution 4.0 International License.
Authors who publish with this journal agree to the following terms:
1) Authors retain copyright and grant the journal right of first publication with the work simultaneously licensed under a Creative Commons Attribution License that allows others to share the work with an acknowledgement of the work's authorship and initial publication in this journal.
2) Authors are able to enter into separate, additional contractual arrangements for the non-exclusive distribution of the journal's published version of the work (e.g., post it to an institutional repository or publish it in a book), with an acknowledgement of its initial publication in this journal.
3) Authors are permitted and encouraged to post their work online (e.g., in institutional repositories or on their website) prior to and during the submission process, as it can lead to productive exchanges, as well as earlier and greater citation of published work.