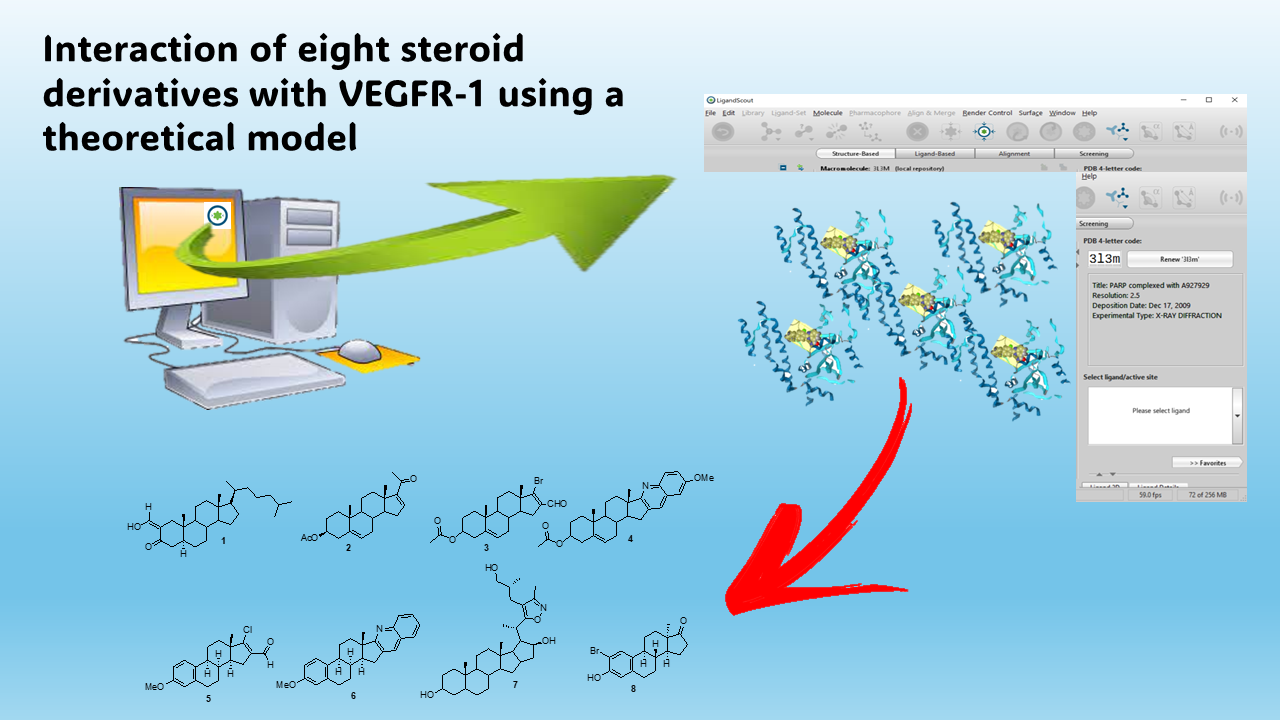
Interaction of eight steroid derivatives with VEGFR-1 using a theoretical model
DOI:
https://doi.org/10.14295/bjs.v3i3.523Keywords:
cancer, steroid, VEGFR-1, docking, theoretical modelAbstract
Some vascular endothelial growth factor receptor-1 (VEGFR-1) inhibitors drugs have been used to cancer cells; however, their interaction with VEGFR-1 is very confusing. The objective of this research was to evaluate the possible interaction of eight steroid derivatives with VEGFR-1 surface using 3hgn protein, cabozantinib, pazopanib, regorafenib, and sorafenib as theoretical tools in DockingServer program. The results showed some differences in the interaction of the steroid derivatives (1-8) with the 3hng protein surface such as i) differences in the number of amino acids; ii) different position of some amino acids compared to cabozantinib, pazopanib, regorafenib, and sorafenib. Besides, the inhibition constant (Ki) for steroid derivatives 1, 3, 6 and 8 was lower compared to cabozantinib and sorafenib drugs. In addition, other data display that Ki for steroid analogs 1, 3, 4, 6, 7 and 8 was lower compared with pazopanib and regorafenib. In conclusion, all these data suggest that steroid derivatives 1, 3, 4, 6, 7 and 8 could act as VEGFR-1 inhibitors and this phenomenon could be translated as good compounds to treat cancer cells.
References
Atzori, M., Ceci, C., Ruffini, F., Trapani, M., Barbaccia, M., Tentori, L., D’Atri, S., Lacal, P. M., Graziani, G. (2020). Role of VEGFR‐1 in melanoma acquired resistance to the BRAF inhibitor vemurafenib. Journal of Cellular and Molelcular Medicine, 24(1): 465-475. https://doi.org/10.1111/jcmm.14755 DOI: https://doi.org/10.1111/jcmm.14755
Banerjee, P., Eckert, A., Schrey, A., & Preissner, R. (2018). ProTox-II: a webserver for the prediction of toxicity of chemicals. Nucleic Acids Research, 46(W1), W257-W263. https://doi.org/10.1093/nar/gky318 DOI: https://doi.org/10.1093/nar/gky318
Banerjee, S., Velásquez-Zapata, V., Fuerst, G., Elmore, J., & Wise, R. (2021). NGPINT: a next-generation protein–protein interaction software. Briefings in Bioinformatics, 22(4), 1-14. https://doi.org/10.1093/bib/bbaa351 DOI: https://doi.org/10.1093/bib/bbaa351
Bekaii-Saab, T., Ou, F., Ahn, D., Boland, P., Ciombor, K., & Heying, E. (2019). Regorafenib dose-optimisation in patients with refractory metastatic colorectal cancer (ReDOS): a randomised, multicentre, open-label, phase 2 study. The Lancet Oncology, 20(8), 1070-1082. https://doi.org/10.1016/S1470-2045(19)30272-4 DOI: https://doi.org/10.1016/S1470-2045(19)30272-4
Bianco, R., Rosa, R., Damiano, V., Daniele, G., Gelardi, T., & Garofalo, S. (2008). Vascular endothelial growth factor
receptor-1 contributes to resistance to anti-epidermal growth factor receptor drugs in human cancer cells. Clinical Cancer Research, 14(16), 5069-5080. DOI: https://doi.org/10.1158/1078-0432.CCR-07-4905
Borba, J., Alves, V., Braga, R., Korn, D., Overdahl, K., Silva, A. (2022). STopTox: An in silico alternative to animal testing for acute systemic and topical toxicity. Environmental Health Perspectives, 130(2), 027012.
https://doi.org/10.1289/EHP9341 DOI: https://doi.org/10.1289/EHP9341
Bouïs, D., Hospers, G., Meijer, C. (2001). Endothelium in vitro: a review of human vascular endothelial cell lines for blood vessel-related research. Angiogenesis, 4, 91-102. https://doi.org/10.1023/A:1012259529167 DOI: https://doi.org/10.1023/A:1012259529167
Bruix, J., Qin, S., Merle, P., Granito, A., Huang, Y. H., & Bodoky, G. (2016). Regorafenib for patients with hepatocellular carcinoma who progressed on sorafenib treatment (RESORCE): a randomised, double-blind, placebo-controlled, phase 3 trial. The Lancet, 389: 56-66. https://doi.org/10.1016/S0140-6736(16)32453-9 DOI: https://doi.org/10.1016/S0140-6736(16)32453-9
Campani, C., Rimassa, L., Personeni, N., & Marra, F. (2020). Angiogenesis inhibitors for advanced hepatocellular carcinoma: in search for the right partner. Annals of Translational Medicine, 8(22), 1532. https://doi.org/10.21037%2Fatm-20-3788 DOI: https://doi.org/10.21037/atm-20-3788
Carmeliet, P. (2005). VEGF as a key mediator of angiogenesis in cancer. Oncology, 69, 4-10. http://dx.doi.org/10.1159%2F000088478 DOI: https://doi.org/10.1159/000088478
Chui, C. (2010). The LogP and MLogP models for parallel image processing with multi-core microprocessor. Proceendings of the Sympposium on Information and Communication Technology, 23-27. https://doi.org/10.1145/1852611.1852616 DOI: https://doi.org/10.1145/1852611.1852616
Daina, A., Michielin, O., & Zoete, V. (2014). iLOGP: a simple, robust, and efficient description of n-octanol/water partition coefficient for drug design using the GB/SA approach. Journal of Chemical Information and Modeling, 54(12), 3284-3301. https://doi.org/10.1021/ci500467k DOI: https://doi.org/10.1021/ci500467k
Daina, A., & Zoete, V. (2016). A boiled‐egg to predict gastrointestinal absorption and brain penetration of small molecules. ChemMedChem, 11(11), 1117-1121. https://doi.org/10.1002/cmdc.201600182 DOI: https://doi.org/10.1002/cmdc.201600182
Derendorf, H., & Meibohm, B. (1999). Modeling of pharmacokinetic/pharmacodynamic (PK/PD) relationships: concepts and perspectives. Pharmaceutical Research, 16, 176-185. https://doi.org/10.1023/A:1011907920641 DOI: https://doi.org/10.1023/A:1011907920641
Figueroa-Valverde, L., Rosas-Nexticapa, M., Alvarez-Ramirez, M., López-Ramos, M., Díaz-Cedillo, F., & Mateu-Armad, M. (2023). Evaluation of biological activity exerted by Dibenzo [b, e] Thiophene-11 (6H)-One on left ventricular pressure using an isolated rat heart model. Drug Research, 73(05), 263-270. DOI: 10.1055/a-1995-6351 DOI: https://doi.org/10.1055/a-1995-6351
Figueroa-Valverde, L., Rosas-Nexticapa, M., Montserrat, M., Díaz-Cedillo, F., López-Ramo, M., & Alvarez-Ramirez, M. (2023). Synthesis and theoretical interaction of 3-(2-oxabicyclo [7.4. 0] trideca-1 (13), 9, 11-trien-7-yn-12-yloxy)-steroid deriva-tive with 17β-hydroxysteroid dehydrogenase enzyme surface. Biointerface Research in Applied Chemistry, 13(3), 1-11. https://doi.org/10.33263/BRIAC133.266 DOI: https://doi.org/10.33263/BRIAC133.266
Forli, S., Huey, R., Pique, M., Sanner, M., Goodsell, D., & Olson, A. (2016). Computational protein–ligand docking and virtual drug screening with the AutoDock suite. Nature Protocols, 11(5), 905-919. https://doi.org/10.1038/nprot.2016.051 DOI: https://doi.org/10.1038/nprot.2016.051
Ge, L., Xun, C., & Li, W. (2021). Extracellular vesicles derived from hypoxia preconditioned olfactory mucosa mesenchymal stem cells enhance angiogenesis via miR-612. Journal of Nanobiotechnology, 19, 1-23. https://doi.org/10.1186/s12951-021-01126-6 DOI: https://doi.org/10.1186/s12951-021-01126-6
Grosser, G., Baringhaus, K., Döring, B., Kramer, W., Petzinger, E., & Geyer, J. (2016). Identification of novel inhibitors of the steroid sulfate carrier ‘sodium-dependent organic anion transporter’SOAT (SLC10A6) by pharmacophore modelling. Molecular and Cellular Endocrinology, 428, 133-141. https://doi.org/10.1016/j.mce.2016.03.028 DOI: https://doi.org/10.1016/j.mce.2016.03.028
Hassan-Baig, M., Ahmad, K., Roy, S., Mohammad-Ashraf, J., Adil, M., Haris-Siddiqui, M., & Choi, I. (2016). Computer aided drug design: success and limitations. Current Pharmaceutical Design, 22(5), 572-581. DOI: https://doi.org/10.2174/1381612822666151125000550
Kanacher, T., Lindauer, A., Mezzalana, E., Michon, I., Veau, C., & Mantilla, J. (2020). A physiologically-based pharmacokinetic (PBPK) model network for the prediction of CYP1A2 and CYP2C19 drug–drug–gene interactions with fluvoxamine, omeprazole, s-mephenytoin, moclobemide, tizanidine, mexiletine, ethinylestradiol, and caffeine. Pharmaceutics, 12(12), 1191. https://doi.org/10.3390/pharmaceutics12121191 DOI: https://doi.org/10.3390/pharmaceutics12121191
Kelley, R., Rimassa, L., & Cheng, A. (2022). Cabozantinib plus atezolizumab versus sorafenib for advanced hepatocellular carcinoma (COSMIC-312): a multicentre, open-label, randomised, phase 3 trial. The Lancet Oncology, 23, 995-1008. https://doi.org/10.1016/S1470-2045(22)00326-6 DOI: https://doi.org/10.1016/S1470-2045(22)00326-6
Khruschev, S., Abaturova, A., Diakonova, A., Ustinin, D., Zlenko, D., & Fedorov, V. (2013). Multi-particle Brownian dynamics software ProKSim for protein-protein interactions modeling. Computer Research and Modeling, 5(1), 47-64. https://doi.org/10.20537/2076-7633-2013-5-1-47-64 DOI: https://doi.org/10.20537/2076-7633-2013-5-1-47-64
Klasa-Mazurkiewicz, D., Jarząb, M., Milczek, T., Lipińska, B., & Emerich, J. (2011). Clinical significance of VEGFR-2 and VEGFR-3 expression in ovarian cancer patients. Polish Journal of Pathology, 62(1), 31-40.
Kopparapu, P., Boorjian, S., Robinson, B., Downes, M., Gudas, L., & Mongan, N. (2013). Expression of VEGF and its receptors VEGFR1/VEGFR2 is associated with invasiveness of bladder cancer. Anticancer Research, 33(6), 2381-2390.
Lagunin, A., Zakharov, A., Filimonov, D., & Poroikov, V. (2011). QSAR modelling of rat acute toxicity on the basis of PASS prediction. Molecular Informatics, 30(2‐3), 241-250. https://doi.org/10.1002/minf.201000151 DOI: https://doi.org/10.1002/minf.201000151
Lee, A., Jones, R., & Huang, P. (2019). Pazopanib in advanced soft tissue sarcomas. Signal Transduction and Targeted Therapy, 4(1), 1-9. https://doi.org/10.1038/s41392-019-0049-6 DOI: https://doi.org/10.1038/s41392-019-0049-6
Lee, H., Xu, Y., & He, L. (2021). Role of venous endothelial cells in developmental and pathologic angiogenesis. Circulation, 144, 1308-1322. https://doi.org/10.1161/CIRCULATIONAHA.121.054071 DOI: https://doi.org/10.1161/CIRCULATIONAHA.121.054071
Levitt, D. (2002). PKQuest: capillary permeability limitation and plasma protein binding–application to human inulin, dicloxacillin and ceftriaxone pharmacokinetics. BMC Clinical Pharmacology, 2(1), 1-11. https://doi.org/10.1186/1472-6904-2-7 DOI: https://doi.org/10.1186/1472-6904-2-7
Lo, J., Lau, E., Ching, R., Cheng, B., Ma, M., Ng, I., & Lee, T. (2015). Nuclear factor kappa B–mediated CD47 up‐regulation promotes sorafenib resistance and its blockade synergizes the effect of sorafenib in hepatocellular carcinoma in mice. Hepatology, 62(2), 534-545. https://doi.org/10.1002/hep.27859 DOI: https://doi.org/10.1002/hep.27859
Macalino, S., Gosu, V., Hong, S., & Choi, S. (2015). Role of computer-aided drug design in modern drug discovery. Archives of Pharmacal Research, 38, 1686-1701. https://doi.org/10.1007/s12272-015-0640-5 DOI: https://doi.org/10.1007/s12272-015-0640-5
Mahanthesh, M., Ranjith, D., Yaligar, R., Jyothi, R., Narappa, G., & Ravi, M. (2020). Swiss ADME prediction of phytochemicals present in Butea monosperma (Lam.) Taub. Journal of Pharmacognosy and Phytochemistry, 9(3), 1799-1809.
Matsuzaki, Y., Uchikoga, N., Ohue, M., Shimoda, T., Sato, T., & Ishida, T. (2013). MEGADOCK 3.0: a high-performance protein-protein interaction prediction software using hybrid parallel computing for petascale supercomputing environments. Source Code for Biology and Medicine, 8(1), 1-8. https://doi.org/10.1186/1751-0473-8-18 DOI: https://doi.org/10.1186/1751-0473-8-18
Mezquita, B., Pineda, E., Mezquita, J., Mezquita, P., Pau, M., Codony‐Servat, J. (2016). LoVo colon cancer cells resistant to oxaliplatin overexpress c‐MET and VEGFR‐1 and respond to VEGF with dephosphorylation of c‐MET. Molecular Carcinogenesis, 55(5), 411-419. https://doi.org/10.1002/mc.22289 DOI: https://doi.org/10.1002/mc.22289
Mezu-Ndubuisi, O., & Maheshwari, A. (2021). The role of integrins in inflammation and angiogenesis. Pediatric Research, 89, 1619-1626. https://doi.org/10.1038/s41390-020-01177-9 DOI: https://doi.org/10.1038/s41390-020-01177-9
Mir, N., Jayachandran, A., Dhungel, B., Shrestha, R., & Steel, J. (2017). Epithelial-to-mesenchymal transition: A mediator of sorafenib resistance in advanced hepatocellular carcinoma. Current Cancer Drug Targets, 17(8), 698-706. https://doi.org/10.2174/1568009617666170427104356 DOI: https://doi.org/10.2174/1568009617666170427104356
Nagano, H., Tomida, C., Yamagishi, N., Teshima-Kondo, S. (2019). VEGFR-1 regulates EGF-R to promote proliferation in
colon cancer cells. International Journal of Molecular Sciences, 20(22), 5608. https://doi.org/10.3390/ijms20225608 DOI: https://doi.org/10.3390/ijms20225608
Neves, M., Dinis, T., Colomb, G., De-Melo., M. (2009). An efficient steroid pharmacophore-based strategy to identify new aromatase inhibitors. European Journal of Medicinal Chemistry, 44(10), 4121-4127. https://doi.org/10.1016/j.ejmech.2009.05.003 DOI: https://doi.org/10.1016/j.ejmech.2009.05.003
Pavlakis, N., Sjoquist, K., Martin, A., Tsobanis, E., Yip, S., Kang, Y. K., & Goldstein, D. (2016). Regorafenib for the treatment of advanced gastric cancer (INTEGRATE): a multinational placebo-controlled phase II trial. Journal of Clinical Oncology, 34(23), 2728-2735. https://doi.org/10.1200%2FJCO.2015.65.1901 DOI: https://doi.org/10.1200/JCO.2015.65.1901
Radifar, M., Yuniarti, N., & Istyastono, E. (2013). PyPLIF: Python-based protein-ligand interaction fingerprinting. Bioinformation, 9(6), 325-328. https://doi.org/10.6026%2F97320630009325 DOI: https://doi.org/10.6026/97320630009325
Rahimi, N., Dayanir, V., & Lashkari, K. (2000). Receptor chimeras indicate that the vascular endothelial growth factor receptor-1 (VEGFR-1) modulates mitogenic activity of VEGFR-2 in endothelial cells. Journal of Biological Chemistry, 275(22), 16986-16992. https://doi.org/10.1074/jbc.M000528200 DOI: https://doi.org/10.1074/jbc.M000528200
Salentin, S., Schreiber, S., Haupt, V., Adasme, M., & Schroeder, M. (2015). PLIP: fully automated protein–ligand interaction profiler. Nucleic Acids Research, 43(W1), W443-W447. https://doi.org/10.1093/nar/gkv315 DOI: https://doi.org/10.1093/nar/gkv315
Saxena, A., Devillers, J., Pery, A., Beaudouin, R., Balaramnavar, V., & Ahmed, S. (2014). Modelling the binding affinity of steroids to zebrafish sex hormone-binding globulin. SAR and QSAR in Environmental Research, 25(5), 407-421. https://doi.org/10.1080/1062936X.2014.909197 DOI: https://doi.org/10.1080/1062936X.2014.909197
Seidel, T., Bryant, S., Ibis, G., Poli, G., & Langer, T. (2017). 3D Pharmacophore modeling techniques in computer-aided molecular design using ligandscout. Tutorials in Chemoinformatics, 279-309. https://doi.org/10.1002/9781119161110.ch20 DOI: https://doi.org/10.1002/9781119161110.ch20
Shah, A. (2022). Pharmacokinetic modeling program (PKMP): A software for PK/PD data analysis. Pharmacokinetics and Pharmacodynamics of Nanoparticulate Drug Delivery Systems, 101-139. https://doi.org/10.1007/978-3-030-83395-4_7 DOI: https://doi.org/10.1007/978-3-030-83395-4_7
Shahryari, S., Mohammadnejad, P., Noghabi, K. (2021). Screening of anti-Acinetobacter baumannii phytochemicals, based on the potential inhibitory effect on OmpA and OmpW functions. Royal Society Open Science, 8(8), 201652. https://doi.org/10.1098/rsos.201652 DOI: https://doi.org/10.1098/rsos.201652
Shibuya, M. (2006). Vascular endothelial growth factor receptor-1 (VEGFR-1/Flt-1): a dual regulator for angiogenesis. Angiogenesis, 4, 225-230. https://doi.org/10.1007/s10456-006-9055-8 DOI: https://doi.org/10.1007/s10456-006-9055-8
Shiri, P., Ramezanpour, S., & Amani, A. (2022). A patent review on efficient strategies for the total synthesis of pazopanib, regorafenib and lenvatinib as novel anti-angiogenesis receptor tyrosine kinase inhibitors for cancer therapy. Molecular Diversity, 26, 2981-3002. https://doi.org/10.1007/s11030-022-10406-8 DOI: https://doi.org/10.1007/s11030-022-10406-8
Silva, S., Bowen, K., Rychahou, P., Jackson, L., Weiss, H., & Lee, E. (2011). VEGFR‐2 expression in carcinoid cancer cells and its role in tumor growth and metastasis. International Journal of Cancer, 128(5), 1045-1056. https://doi.org/10.1002/ijc.25441 DOI: https://doi.org/10.1002/ijc.25441
Stăncioiu, L., Gherman, A., & Brezeștean, I. (2022). Vibrational spectral analysis of Sorafenib and its molecular docking study compared to other TKIs. Journal of Molecular Structure, 1248, 131507. https://doi.org/10.1016/j.molstruc.2021.131507 DOI: https://doi.org/10.1016/j.molstruc.2021.131507
Temml, V., Kaserer, T., Kutil, Z., Landa, P., Vanek, T., & Schuster, D. (2014). Pharmacophore modeling for COX-1 and-2 inhibitors with LigandScout in comparison to discovery studio. Future Medicinal Chemistry, 6(17), 1869-1881. https://doi.org/10.4155/fmc.14.114 DOI: https://doi.org/10.4155/fmc.14.114
Tomida, C., Nagano, H., Yamagishi, N., Uchida, T., Ohno, A., Hirasaka, K. (2017). Regorafenib induces adaptive resistance of colorectal cancer cells via inhibition of vascular endothelial growth factor receptor. Journal of Medical
Investigation, 64(3.4), 262-265. https://doi.org/10.2152/jmi.64.262 DOI: https://doi.org/10.2152/jmi.64.262
Tresaugues, L., Roos, A., Arrowsmith, C., Berglund, H., Bountra, C., Collins, R., Nordlund, P. (2009). Crystal structure of VEGFR1 in complex with N-(4-Chlorophenyl)-2-((pyridin-4-ylmethyl) amino) benzamide. 2013; RCSB Protein Data Bank. https://doi.org/10.2210/pdb3HNG/pdb DOI: https://doi.org/10.2210/pdb3hng/pdb
Vane, J., Änggård, E., & Botting. R. (1990). Regulatory functions of the vascular endothelium. The New England Journal of Medicine, 323, 27-36. DOI: 10.1056/NEJM199007053230106 DOI: https://doi.org/10.1056/NEJM199007053230106
Wallace, A., Laskowski, R., Thornton, J. (1995). LIGPLOT: a program to generate schematic diagrams of protein-ligand interactions. Protein Engineering, Design & Selection, 8(2), 127-134. https://doi.org/10.1093/protein/8.2.127 DOI: https://doi.org/10.1093/protein/8.2.127
Wang, X., Shen, Y., Wang, S., Li, S., Zhang, W., Liu, X., Li, H. (2017). PharmMapper 2017 update: a web server for potential drug target identification with a comprehensive target pharmacophore database. Nucleic Acids Research, 45(W1), W356-W360. https://doi.org/10.1093/nar/gkx374 DOI: https://doi.org/10.1093/nar/gkx374
Yonemura, Y., Fushida, S., Bando, E., Kinoshita, K., Miwa, K., Endo, Y., & Sasaki, T. (2001). Lymphangiogenesis and the vascular endothelial growth factor receptor (VEGFR)-3 in gastric cancer. European Journal of Cancer, 37(7), 918-923. https://doi.org/10.1016/S0959-8049(01)00015-6 DOI: https://doi.org/10.1016/S0959-8049(01)00015-6
Zhang, Y., Wang, Y., & Lei, Z. (2019). Regorafenib antagonizes BCRP-mediated multidrug resistance in colon cancer. Cancer Letters, 442, 104-112. https://doi.org/10.1016/j.canlet.2018.10.032 DOI: https://doi.org/10.1016/j.canlet.2018.10.032
Zhao, Y., Guo, S., & Deng, J. (2022). VEGF/VEGFR-targeted therapy and immunotherapy in non-small cell lung cancer: targeting the tumor microenvironment. International Journal of Biological Sciences, 18(9), 3845-3858. https://doi.org/10.7150%2Fijbs.70958 DOI: https://doi.org/10.7150/ijbs.70958
Zhong, T., Hao, Y., Yao, X., Zhang, S., Duan, X., Yin, Y., & Zhang, X. (2018). Effect of XlogP and Hansen solubility parameters on small molecule modified paclitaxel anticancer drug conjugates self-assembled into nanoparticles. Bioconjugate Chemistry, 29(2), 437-444. https://doi.org/10.1021/acs.bioconjchem.7b00767 DOI: https://doi.org/10.1021/acs.bioconjchem.7b00767
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2024 Maria Lopez-Ramos, Lauro Figueroa-Valverde, Magdalena Alvarez-Ramirez, Marcela Rosas-Nexicapa, Maria Virginia Mateu-Armand, Regina Cauich-Carrillo

This work is licensed under a Creative Commons Attribution 4.0 International License.
Authors who publish with this journal agree to the following terms:
1) Authors retain copyright and grant the journal right of first publication with the work simultaneously licensed under a Creative Commons Attribution License that allows others to share the work with an acknowledgement of the work's authorship and initial publication in this journal.
2) Authors are able to enter into separate, additional contractual arrangements for the non-exclusive distribution of the journal's published version of the work (e.g., post it to an institutional repository or publish it in a book), with an acknowledgement of its initial publication in this journal.
3) Authors are permitted and encouraged to post their work online (e.g., in institutional repositories or on their website) prior to and during the submission process, as it can lead to productive exchanges, as well as earlier and greater citation of published work.