Occupational therapy for individuals with chronic kidney disease undergoing renal rehabilitation: A literature review
DOI:
https://doi.org/10.14295/bjs.v3i10.643Keywords:
chronic kidney disease, hemodialysis, occupational therapy, activities of daily livingAbstract
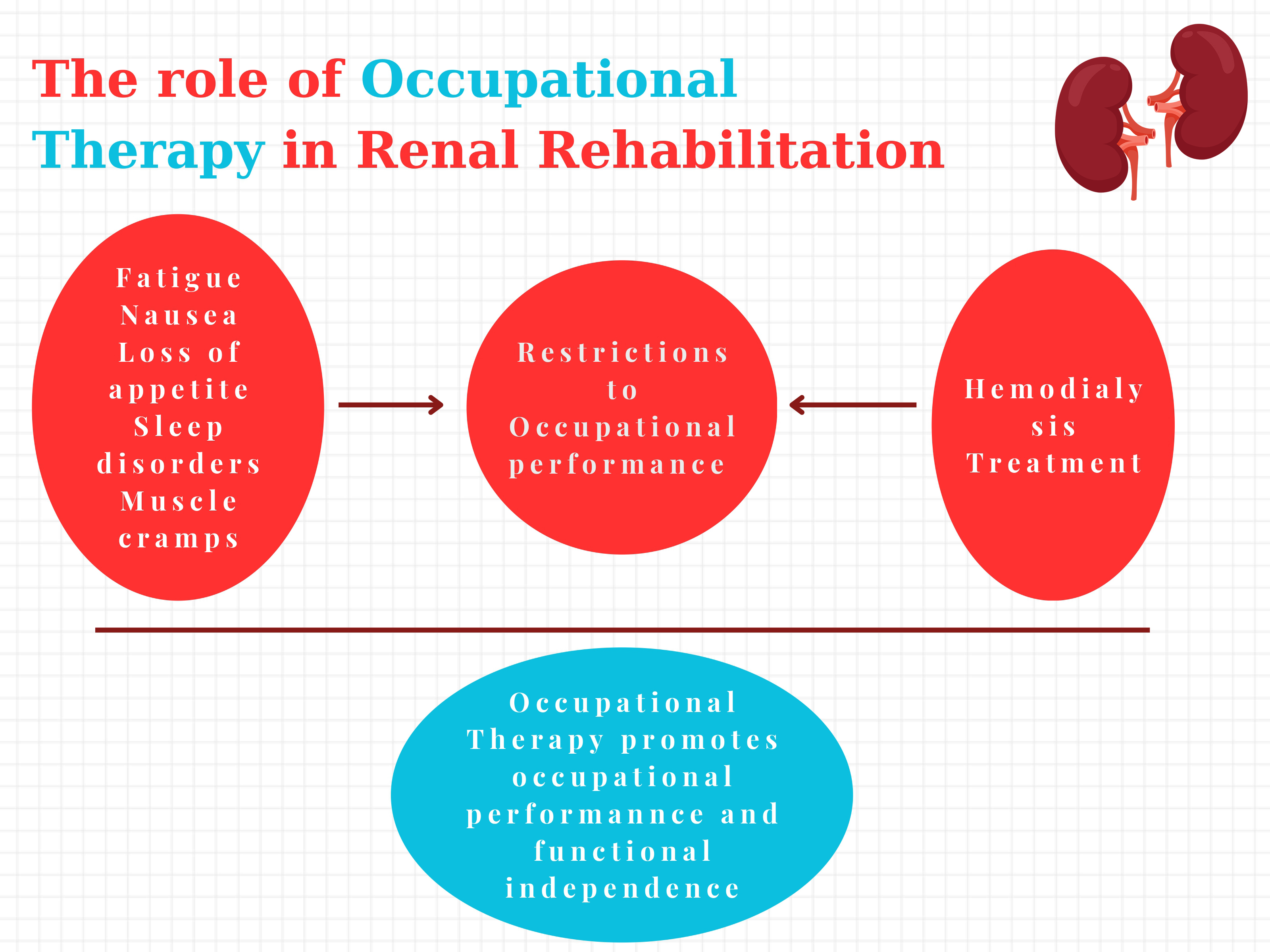
Chronic kidney disease is a life-changing condition affecting 10% of the global population, leading to significant health challenges in a person’s daily life. It is considered a worldwide health crisis due to its increasing prevalence in the general population and the development of complicated clinical symptoms if left untreated. Hemodialysis is a treatment procedure that helps substitute renal function, which is vital for the individual's health. Most health-related scientific literature focuses on understanding the underlying mechanisms of the disease, advancing hemodialysis treatment, and minimizing adverse side effects. Meanwhile, another scientific direction aims to evaluate the functioning and quality of life of these individuals, who can, in some cases, become extremely debilitated. People with chronic kidney disease undergoing hemodialysis often experience a significant disruption in their ability and efficiency to perform meaningful tasks and established routines independently. Occupational therapy can help empower individuals with chronic kidney disease undergoing hemodialysis, enabling life participation while minimizing the burden and health-related consequences of the disease.
References
American Occupational Therapy Association. (2020). Occupational therapy practice framework: Domain and Process. American Journal of Occupational Therapy, 74(4). https://doi.org/10.5014/ajot.2020.74s2001 DOI: https://doi.org/10.5014/ajot.2020.74S2001
Anderton, N., Giri, A., Wei, G., Marcus, R. L., Chen, H., Bjordahl, T., Habib, A. N., Herrera, J., & Srinivasan Beddhu. (2015). Sedentary behavior in individuals with diabetic chronic kidney disease and maintenance hemodialysis. Journal of Renal Nutrition, 25(4), 364-370. https://doi.org/10.1053/j.jrn.2015.01.018 DOI: https://doi.org/10.1053/j.jrn.2015.01.018
Angulo, J., El Assar, M., Álvarez-Bustos, A., & Rodríguez-Mañas, L. (2020). Physical activity and exercise: Strategies to
manage frailty. Redox Biology, 35, 101513. https://doi.org/10.1016/j.redox.2020.101513 DOI: https://doi.org/10.1016/j.redox.2020.101513
Brodski, J., Rossell, S. L., Castle, D. J., & Tan, E. J. (2019). A systematic review of cognitive impairments associated with kidney failure in adults before natural age-related changes. Journal of the International Neuropsychological Society, 25(1), 101-114. https://doi.org/10.1017/S1355617718000917 DOI: https://doi.org/10.1017/S1355617718000917
Bronas, U. G., Puzantian, H., & Hannan, M. (2017). Cognitive impairment in chronic kidney disease: Vascular milieu and the potential therapeutic role of exercise. BioMed Research International, 1-10. https://doi.org/10.1155/2017/2726369 DOI: https://doi.org/10.1155/2017/2726369
Burns, C. M., Knopman, D. S., Tupper, D. E., Davey, C. S., Slinin, Y. M., Lakshminarayan, K., Rossom, R. C., Pederson, S. L., Gilbertson, D. T., & Murray, A. M. (2017). Prevalence and risk of severe cognitive impairment in advanced chronic kidney disease. The Journals of Gerontology: Series A, 73(3), 393-399. https://doi.org/10.1093/gerona/glx241 DOI: https://doi.org/10.1093/gerona/glx241
Castle, E. M., Billany, R. E., Lightfoot, C. J., Annema, C., De Smet, S., Graham-Brown, M. P. M., & Greenwood, S. A. (2023). Exercise as a therapeutic intervention in chronic kidney disease: are we nearly there yet? Current Opinion in Nephrology and Hypertension, 32(6), 502-508. https://doi.org/10.1097/mnh.0000000000000923 DOI: https://doi.org/10.1097/MNH.0000000000000923
Cha, J., & Han, D. (2020). Health-Related Quality of Life Based on Comorbidities Among Patients with End-Stage Renal Disease. Osong Public Health and Research Perspectives, 11(4), 194-200. https://doi.org/10.24171/j.phrp.2020.11.4.08 DOI: https://doi.org/10.24171/j.phrp.2020.11.4.08
Chang, J., Hou, W.-W., Wang, Y.-F., & Sun, Q.-M. (2020). Main risk factors related to activities of daily living in non-dialysis patients with chronic kidney disease stage 3–5: A case–control study. Clinical Interventions in Aging, 15, 609-618. https://doi.org/10.2147/cia.s249137 DOI: https://doi.org/10.2147/CIA.S249137
Chu, N. M., Sison, S., Muzaale, A. D., Haugen, C. E., Garonzik-Wang, J. M., Brennan, D. C., Norman, S. P., Segev, D. L., & McAdams-DeMarco, M. (2019). Functional independence, access to kidney transplantation and waitlist mortality. Nephrology Dialysis Transplantation, 35(5), 870-877. https://doi.org/10.1093/ndt/gfz265 DOI: https://doi.org/10.1093/ndt/gfz265
Clarkson, M. J., Bennett, P. N., Fraser, S. F., & Warmington, S. A. (2019). Exercise interventions for improving objective physical function in patients with end-stage kidney disease on dialysis: a systematic review and meta-analysis. American Journal of Physiology-Renal Physiology, 316(5), F856-F872. https://doi.org/10.1152/ajprenal.00317.2018 DOI: https://doi.org/10.1152/ajprenal.00317.2018
Cotterell, N., Buffel, T., & Phillipson, C. (2018). Preventing social isolation in older people. Maturitas, 113(1), 80–84. https://doi.org/10.1016/j.maturitas.2018.04.014 DOI: https://doi.org/10.1016/j.maturitas.2018.04.014
de Vries, E. F., Los, J., de Wit, G. A., & Hakkaart - van Roijen, L. (2021). Patient, family and productivity costs of end-stage renal disease in the Netherlands; exposing non-healthcare related costs. BMC Nephrology, 22(1). https://doi.org/10.1186/s12882-021-02548-y DOI: https://doi.org/10.1186/s12882-021-02548-y
Donnelly, C., O’Neill, C., Bauer, M., & Letts, L. (2017). Canadian occupational performance measure (COPM) in primary care: A profile of practice. American Journal of Occupational Therapy, 71(6), 7106265010p1. https://doi.org/10.5014/ajot.2017.020008 DOI: https://doi.org/10.5014/ajot.2017.020008
Endo, M., Nakamura, Y., Murakami, T., Tsukahara, H., Watanabe, Y., Matsuoka, Y., Ohsawa, I., Gotoh, H., Inagaki, T., & Oguchi, E. (2017). Rehabilitation improves prognosis and activities of daily living in hemodialysis patients with low activities of daily living. Physical Therapy Research, 20(1), 9-15. https://doi.org/10.1298/ptr.e9898 DOI: https://doi.org/10.1298/ptr.E9898
Fang, H.-Y., Burrows, B. T., King, A. C., & Wilund, K. R. (2020). A comparison of intradialytic versus out-of-clinic exercise training programs for hemodialysis patients. Blood Purification, 49(1-2), 151-157. https://doi.org/10.1159/000503772 DOI: https://doi.org/10.1159/000503772
Fotaraki, Z.-M., Gerogianni, G., Vasilopoulos, G., Polikandrioti, M., Giannakopoulou, N., & Alikari, V. (2022). Depression, adherence, and functionality in patients undergoing hemodialysis. Cureus, 14(2).
https://doi.org/10.7759/cureus.21872 DOI: https://doi.org/10.7759/cureus.21872
Goto, Y. (2017). Renal rehabilitation in occupational therapy for patients with chronic kidney disease. Physical Medicine and Rehabilitation Research, 2(5), 1-3. https://doi.org/10.15761/PMRR.1000S1001
Graver, A., Odell, M., Churilov, L., Power, D. A., Mount, P. F., Davies, M., Choy, S., Paizis, K., & Cook, N. (2021). Dialysis and driving: An anonymous survey of patients receiving dialysis for end stage kidney disease. Internal Medicine Journal, 51(10), 1691-1699. https://doi.org/10.1111/imj.15198 DOI: https://doi.org/10.1111/imj.15198
Hamzi, M., Hassani, K., Asseraji, M., & El Kabbaj, D. (2017). Insomnia in hemodialysis patients: A multicenter study from morocco. Saudi Journal of Kidney Diseases and Transplantation, 28(5), 1112. https://doi.org/10.4103/1319-2442.215152 DOI: https://doi.org/10.4103/1319-2442.215152
Himmelfarb, J., Vanholder, R., Mehrotra, R., & Tonelli, M. (2020). The current and future landscape of dialysis. Nature Reviews. Nephrology, 16(16), 1–13. https://doi.org/10.1038/s41581-020-0315-4 DOI: https://doi.org/10.1038/s41581-020-0315-4
Jesus, N. M., Souza, G. F., Mendes-Rodrigues, C., Almeida Neto, O. P., Rodrigues, D. D. M., & Cunha, C. M. (2019). Quality of life of individuals with chronic kidney disease on dialysis. Brazilian Journal of Nephrology, 41(3), 364-374. https://doi.org/10.1590/2175-8239-jbn-2018-0152 DOI: https://doi.org/10.1590/2175-8239-jbn-2018-0152
Kalsoom, U., Khan, S., & Ahmad, I. (2020). Impact of hemodialysis on the wellbeing of chronic kidney diseases patients: a pre-post analysis. Middle East Current Psychiatry, 27(1). https://doi.org/10.1186/s43045-020-00060-x DOI: https://doi.org/10.1186/s43045-020-00060-x
Kasbia, G. S., Farragher, J., Kim, S. J., Famure, O., & Jassal, S. V. (2014). A cross-sectional study examining the functional independence of elderly individuals with a functioning kidney transplant. Transplantation, 98(8), 864-870. https://doi.org/10.1097/tp.0000000000000126 DOI: https://doi.org/10.1097/TP.0000000000000126
Kielhofner, G. (2008). Model of Human occupation: Theory and Application (4th ed.). Lippincott Williams & Wilkins.
Kirkeskov, L., Carlsen, R. K., Lund, T., & Buus, N. H. (2021). Employment of patients with kidney failure treated with dialysis or kidney transplantation—a systematic review and meta-analysis. BMC Nephrology, 22(1). https://doi.org/10.1186/s12882-021-02552-2 DOI: https://doi.org/10.1186/s12882-021-02552-2
Kobayashi, L. C., & Steptoe, A. (2018). Social isolation, loneliness, and health behaviors at older ages: Longitudinal cohort study. Annals of Behavioral Medicine, 52(7), 582-593. https://doi.org/10.1093/abm/kax033 DOI: https://doi.org/10.1093/abm/kax033
Kohzuki, M. (2024). Renal rehabilitation: Present and future perspectives. Journal of Clinical Medicine, 13(2), 552-552. https://doi.org/10.3390/jcm13020552 DOI: https://doi.org/10.3390/jcm13020552
Kovesdy, C. P. (2022). Epidemiology of chronic kidney disease: an Update 2022. Kidney International Supplements, 12(1), 7-11. https://doi.org/10.1016/j.kisu.2021.11.003 DOI: https://doi.org/10.1016/j.kisu.2021.11.003
Kutner, N. G., Zhang, R., Huang, Y., & Painter, P. (2015). Gait speed and mortality, hospitalization, and functional status change among hemodialysis patients: A US renal data system special study. American Journal of Kidney Diseases, 66(2), 297-304. https://doi.org/10.1053/j.ajkd.2015.01.024 DOI: https://doi.org/10.1053/j.ajkd.2015.01.024
Lambdin-Pattavina, C., & Pyatak, E. (2022). Occupational therapy’s role in chronic conditions. The American Journal of Occupational Therapy, 76(Supplement 3). https://doi.org/10.5014/ajot.2022.76s3003 DOI: https://doi.org/10.5014/ajot.2022.76S3003
Law, M., Baptiste, S., & Carswell, A. (2015). Canadian Occupational Performance Measure (5th ed.). CAOT Publications ACE.
Lewis, R. A., Bohm, C., Fraser, F., Fraser, R., Woytkiw, L., Jurgutis, S., Rubin, M., Smith, G., Buenafe, J., Verdin, N., Hutton, J., & Tonelli, M. (2023). Transportation burden associated with hemodialysis in Canada: A qualitative study of stakeholders. Kidney Medicine, 5(2), 100571. https://doi.org/10.1016/j.xkme.2022.100571 DOI: https://doi.org/10.1016/j.xkme.2022.100571
Liu, Y., Ma, W., Li, M., Han, P., Cai, M., Wang, F., Wang, J., Chen, X., Shi, J., Zhang, X., Zheng, Y., Chen, M., Guo, Q., & Yu, Y. (2021). Relationship between physical performance and mild cognitive impairment in Chinese community-dwelling older adults. Clinical Interventions in Aging, 16, 119-127. https://doi.org/10.2147/cia.s288164 DOI: https://doi.org/10.2147/CIA.S288164
Lu, J. L., Freire, A. X., Molnar, M. Z., Kalantar-Zadeh, K., & Kovesdy, C. P. (2018). Association of chronic insomnia with mortality and adverse renal outcomes. Mayo Clinic Proceedings, 93(11), 1563-1570. https://doi.org/10.1016/j.mayocp.2018.05.032 DOI: https://doi.org/10.1016/j.mayocp.2018.05.032
MacRae, C., Mercer, S. W., Guthrie, B., & Henderson, D. (2020). Comorbidity in chronic kidney disease: a large cross-sectional study of prevalence in Scottish primary care. British Journal of General Practice, 71(704), e243-e249. https://doi.org/10.3399/bjgp20x714125 DOI: https://doi.org/10.3399/bjgp20X714125
Martins, P., Marques, E. A., Leal, D. V., Ferreira, A., Wilund, K. R., & Viana, J. L. (2021). Association between physical activity and mortality in end-stage kidney disease: a systematic review of observational studies. BMC Nephrology, 22(1). https://doi.org/10.1186/s12882-021-02407-w DOI: https://doi.org/10.1186/s12882-021-02407-w
Matsuzawa, R., Kamitani, T., Roshanravan, B., Fukuma, S., Joki, N., & Fukagawa, M. (2019). Decline in the functional status and mortality in patients on hemodialysis: Results from the Japan dialysis outcome and practice patterns study. Journal of Renal Nutrition, 29(6), 504-510. https://doi.org/10.1053/j.jrn.2018.10.012 DOI: https://doi.org/10.1053/j.jrn.2018.10.012
Mayes, J., Pelagia Koufaki, & Sharlene Anuska Greenwood. (2023). Physical activity, function, and exercise-based rehabilitation for people on dialysis. Elsevier EBooks, 582-589 p. https://doi.org/10.1016/b978-0-323-79135-9.00060-4 DOI: https://doi.org/10.1016/B978-0-323-79135-9.00060-4
McQuoid, J. (2017). Finding joy in poor health: The leisure-scapes of chronic illness. Social Science & Medicine, 183, 88-96. https://doi.org/10.1016/j.socscimed.2017.04.044 DOI: https://doi.org/10.1016/j.socscimed.2017.04.044
Mollaoğlu, M., & Başer, E. (2021). Investigation of Effect on Activities of Daily Living and Symptoms in Hemodilaysis Patients. Nigerian Journal of Clinical Practice, 24(9), 1332-1332. https://doi.org/10.4103/njcp.njcp_281_20 DOI: https://doi.org/10.4103/njcp.njcp_281_20
Moorthi, R. N., & Latham-Mintus, K. (2019). Social isolation in chronic kidney disease and the role of mobility limitation. Clinical Kidney Journal, 12(4), 602-610. https://doi.org/10.1093/ckj/sfy134 DOI: https://doi.org/10.1093/ckj/sfy134
Moreno-Tamayo, K., Manrique-Espinoza, B., Ramírez-García, E., & Sánchez-García, S. (2019). Social isolation undermines quality of life in older adults. International Psychogeriatrics, 32(11), 1-10. https://doi.org/10.1017/s1041610219000310 DOI: https://doi.org/10.1017/S1041610219000310
Morishita, S., Tsubaki, A., & Shirai, N. (2017). Physical function was related to mortality in patients with chronic kidney disease and dialysis. Hemodialysis International, 21(4), 483-489. https://doi.org/10.1111/hdi.12564 DOI: https://doi.org/10.1111/hdi.12564
Nakamura, K., Sasaki, T., Yamamoto, S., Hayashi, H., Ako, S., & Tanaka, Y. (2020). Effects of exercise on kidney and physical function in patients with non-dialysis chronic kidney disease: a systematic review and meta-analysis. Scientific Reports, 10(1). https://doi.org/10.1038/s41598-020-75405-x DOI: https://doi.org/10.1038/s41598-020-75405-x
National Kidney Foundation. (2023). Stages of Chronic Kidney Disease (CKD). National Kidney Foundation. Available in: https://www.kidney.org/atoz/content/stages-chronic-kidney-disease-ckd Access in: 07 July, 2024.
Otobe, Y., Hiraki, K., Hotta, C., Nishizawa, H., Izawa, K. P., Taki, Y., Imai, N., Sakurada, T., & Yugo Shibagaki. (2019). Mild cognitive impairment in older adults with pre‐dialysis patients with chronic kidney disease: Prevalence and association with physical function. Nephrology, 24(1), 50-55. https://doi.org/10.1111/nep.13173 DOI: https://doi.org/10.1111/nep.13173
Pereira, J., de Almeida, M. E. M., Batista, M. P. P., & Toldrá, R. C. (2018). Contributions of occupational therapy in health care of users with chronic renal insufficiency in hospital context. Cadernos Brasileiros de Terapia Ocupacional, 28(2), 575-599. https://doi.org/10.4322/2526-8910.ctoAO1855 DOI: https://doi.org/10.4322/2526-8910.ctoAO1855
Pretto, C. R., Winkelmann, E. R., Hildebrandt, L. M., Barbosa, D. A., Colet, C. de F., Stumm, E. M. F., Pretto, C. R., Winkelmann, E. R., Hildebrandt, L. M., Barbosa, D. A., Colet, C. de F., & Stumm, E. M. F. (2020). Quality of life of chronic kidney patients on hemodialysis and related factors. Revista Latino-Americana de Enfermagem, 28, e3327. https://doi.org/10.1590/1518-8345.3641.3327 DOI: https://doi.org/10.1590/1518-8345.3641.3327
Puchulu, M. B., Nuria Garcia-Fernandez, & Landry, M. J. (2023). Food insecurity and chronic kidney disease: Considerations for practitioners. Journal of Renal Nutrition, 33(5), 691-697. https://doi.org/10.1053/j.jrn.2023.06.001 DOI: https://doi.org/10.1053/j.jrn.2023.06.001
Rani, D., & Kalia, R. (2022). Activities of daily living (ADL) and fatigue among patients undergoing hemodialysis. Nursing & Midwifery Research Journal, 18(2), 88-96. https://doi.org/10.1177/0974150x221085747 DOI: https://doi.org/10.1177/0974150X221085747
Rosa, C. S. C., Bueno, D. R., Souza, G. D., Gobbo, L. A., Freitas, I. F., Sakkas, G. K., & Monteiro, H. L. (2015). Factors associated with leisure-time physical activity among patients undergoing hemodialysis. BMC Nephrology, 16(1). https://doi.org/10.1186/s12882-015-0183-5 DOI: https://doi.org/10.1186/s12882-015-0183-5
Savira, F., Ademi, Z., Wang, B. H., Kompa, A. R., Owen, A. J., Liew, D., & Zomer, E. (2021). The preventable productivity burden of kidney disease in Australia. Journal of the American Society of Nephrology, 32(4), 938-949. https://doi.org/10.1681/asn.2020081148 DOI: https://doi.org/10.1681/ASN.2020081148
Schwartz, J. K., & Smith, R. O. (2017). Integration of medication management into occupational therapy practice. American Journal of Occupational Therapy, 71(4). https://doi.org/10.5014/ajot.2017.015032 DOI: https://doi.org/10.5014/ajot.2017.015032
Sheshadri, A., & Johansen, K. L. (2017). Prehabilitation for the Frail Patient Approaching ESRD. Seminars in Nephrology, 37(2), 159-172. https://doi.org/10.1016/j.semnephrol.2016.12.006 DOI: https://doi.org/10.1016/j.semnephrol.2016.12.006
Shiota, K., & Hashimoto, T. (2016). Promotion and support of physical activity in elderly patients on hemodialysis: a case study. Journal of Physical Therapy Science, 28(4), 1378-1383. https://doi.org/10.1589/jpts.28.1378 DOI: https://doi.org/10.1589/jpts.28.1378
Slaven, A., Hsu, J., Schelling, J. R., Navaneethan, S. D., Rincon-Choles, H., McAdams-DeMarco, M. A., Schachere, M., O’Malley, N., Deluca, J., Lustigova, E., Wang, X., Kusek, J., Porter, A. C., Lash, J. P., Rahman, M., & Horwitz, E. (2021). Social Support in Older Adults With CKD: A Report from the CRIC (chronic renal insufficiency cohort) Study. Kidney Medicine, 3(5), 776-784. https://doi.org/10.1016/j.xkme.2021.04.025 DOI: https://doi.org/10.1016/j.xkme.2021.04.025
Tan, L.-H., Chen, P.-S., Chiang, H.-Y., King, E., Yeh, H.-C., Hsiao, Y.-L., Chang, D. R., Chen, S.-H., Wu, M.-Y., & Kuo, C.-C. (2022). Insomnia and poor sleep in CKD: A systematic review and meta-analysis. Kidney Medicine, 4(5), 100458. https://doi.org/10.1016/j.xkme.2022.100458 DOI: https://doi.org/10.1016/j.xkme.2022.100458
Tricco, A. C., Lillie, E., Zarin, W., O’Brien, K. K., Colquhoun, H., Levac, D., Moher, D., Peters, M. D. J., Horsley, T., Weeks, L., Hempel, S., Akl, E. A., Chang, C., McGowan, J., Stewart, L., Hartling, L., Aldcroft, A., Wilson, M. G., Garritty, C., & Lewin, S. (2018). PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Annals of Internal Medicine, 169(7), 467-473. https://doi.org/10.7326/m18-0850 DOI: https://doi.org/10.7326/M18-0850
van Haalen, H., Jackson, J., Spinowitz, B., Milligan, G., & Moon, R. (2020). Impact of chronic kidney disease and anemia on health-related quality of life and work productivity: analysis of multinational real-world data. BMC Nephrology, 21(1). https://doi.org/10.1186/s12882-020-01746-4 DOI: https://doi.org/10.1186/s12882-020-01746-4
Varela, D., Mallawaarachchi, I., & Blandon, P. (2015). A diagnostic screening tool for identifying safe drivers among dialysis patients. Clinical Nephrology, 83(01), 22-28. https://doi.org/10.5414/cn108218 DOI: https://doi.org/10.5414/CN108218
Varghese, S. A. (2019). Barriers to transportation: A study on patients with end-stage renal disease receiving in-center hemodialysis. Journal of Social Service Research, 46(6), 1-12. https://doi.org/10.1080/01488376.2019.1666080 DOI: https://doi.org/10.1080/01488376.2019.1666080
Viggiano, D., Wagner, C. A., Blankestijn, P. J., Bruchfeld, A., Fliser, D., Fouque, D., Frische, S., Gesualdo, L., Gutiérrez, E., Goumenos, D., Hoorn, E. J., Eckardt, K.-U., Knauß, S., König, M., Malyszko, J., Massy, Z., Nitsch, D., Pesce, F., Rychlík, I., & Soler, M. J. (2019). Mild cognitive impairment and kidney disease: clinical aspects. Nephrology Dialysis
Transplantation, 35(1), 10-17. https://doi.org/10.1093/ndt/gfz051 DOI: https://doi.org/10.1093/ndt/gfz051
Villanego, F., Naranjo, J., Vigara, L. A., Cazorla, J. M., Montero, M. E., García, T., Torrado, J., & Mazuecos, A. (2020). Impact of physical exercise in patients with chronic kidney disease: Systematic review and meta-analysis. Nefrología (English Edition), 40(3), 237-252. https://doi.org/10.1016/j.nefroe.2020.06.012 DOI: https://doi.org/10.1016/j.nefroe.2020.06.012
Viswanath, N., Kumar, K., Satish Haridasan, Parameswaran, S., & Priyamvada, P. S. (2019). Functional status in hemodialysis - A comparative study with FIM, ADLQ and 7D5L instruments. Indian Journal of Nephrology, 29(3), 172-172. https://doi.org/10.4103/ijn.ijn_363_17 DOI: https://doi.org/10.4103/ijn.IJN_363_17
Voltarelli, B. C., & Ruzzi-Pereira, A. (2021). Occupational performance of chronic kidney patients undergoing hemodialysis. Revista Família, Ciclos de Vida E Saúde No Contexto Social, 9(3), 631-641. https://doi.org/10.18554/refacs.v9i3.4475
Vyslysel, G., Barker, D., & Hubbard, I. J. (2021). The Canadian occupational performance measure (COPM) as routine practise in community-based rehabilitation: a retrospective chart review. Archives of Rehabilitation Research and Clinical Translation, 3(3), 100134. https://doi.org/10.1016/j.arrct.2021.100134 DOI: https://doi.org/10.1016/j.arrct.2021.100134
Warsame, F., Ying, H., Haugen, C. E., Thomas, A. G., Crews, D. C., Shafi, T., Jaar, B. G., Chu, N. M., Segev, D. L., & McAdams-DeMarco, M. (2018). Intradialytic activities and health-related quality of life among hemodialysis patients. American Journal of Nephrology, 48(3), 181-189. https://doi.org/10.1159/000492623 DOI: https://doi.org/10.1159/000492623
Watanabe, Y., Nakamura, Y., Murakami, T., Matsuura, H., & Gotoh, H. (2016). Positive effects of high cognitive functions on rehabilitation in hemodialysis patients. Japanese Occupational Therapy Research, 35, 582-591.
World Federation of Occupational Therapists. (2018). Definitions of occupational therapy and member organizations. Available in: https://wfot.org/about/about-occupational-therapy Access in 07 July, 2024.
World Health Organization. (2019). International Classification of Diseases and Related Health Problems (11th ed.). https://icd.who.int/en
Wu, X., Yang, L., Wang, Y., Wang, C., Hu, R., & Wu, Y. (2020). Effects of combined aerobic and resistance exercise on renal function in adult patients with chronic kidney disease: a systematic review and meta-analysis. Clinical Rehabilitation, 34(7), 851-865. https://doi.org/10.1177/0269215520924459 DOI: https://doi.org/10.1177/0269215520924459
Xu, H., Garcia-Ptacek, S., Trevisan, M., Evans, M., Lindholm, B., Eriksdotter, M., & Carrero, J. J. (2021). Kidney function, kidney function decline, and the risk of dementia in older adults. Neurology, 96(24), e2956-e2965. https://doi.org/10.1212/wnl.0000000000012113 DOI: https://doi.org/10.1212/WNL.0000000000012113
Yamamoto, S., Inoue, Y., Kuwahara, K., Miki, T., Nakagawa, T., Honda, T., Yamamoto, S., Hayashi, T., & Mizoue, T. (2021). Leisure-time, occupational, and commuting physical activity and the risk of chronic kidney disease in a working population. Scientific Reports, 11(1), 12308. https://doi.org/10.1038/s41598-021-91525-4 DOI: https://doi.org/10.1038/s41598-021-91525-4
Yu, B., Steptoe, A., Chen, Y., & Jia, X. (2021). Social isolation, rather than loneliness, is associated with cognitive decline in older adults: The China health and retirement longitudinal study. Psychological Medicine, 1-8. https://doi.org/10.1017/s0033291720001026 DOI: https://doi.org/10.1017/S0033291720001026
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2024 Nikolaos Gerosideris, Symeon-Dimitrios Daskalou, Christina Ouzouni, Pinelopi Vlotinou, Ioanna-Giannoula Katsouri

This work is licensed under a Creative Commons Attribution 4.0 International License.
Authors who publish with this journal agree to the following terms:
1) Authors retain copyright and grant the journal right of first publication with the work simultaneously licensed under a Creative Commons Attribution License that allows others to share the work with an acknowledgement of the work's authorship and initial publication in this journal.
2) Authors are able to enter into separate, additional contractual arrangements for the non-exclusive distribution of the journal's published version of the work (e.g., post it to an institutional repository or publish it in a book), with an acknowledgement of its initial publication in this journal.
3) Authors are permitted and encouraged to post their work online (e.g., in institutional repositories or on their website) prior to and during the submission process, as it can lead to productive exchanges, as well as earlier and greater citation of published work.